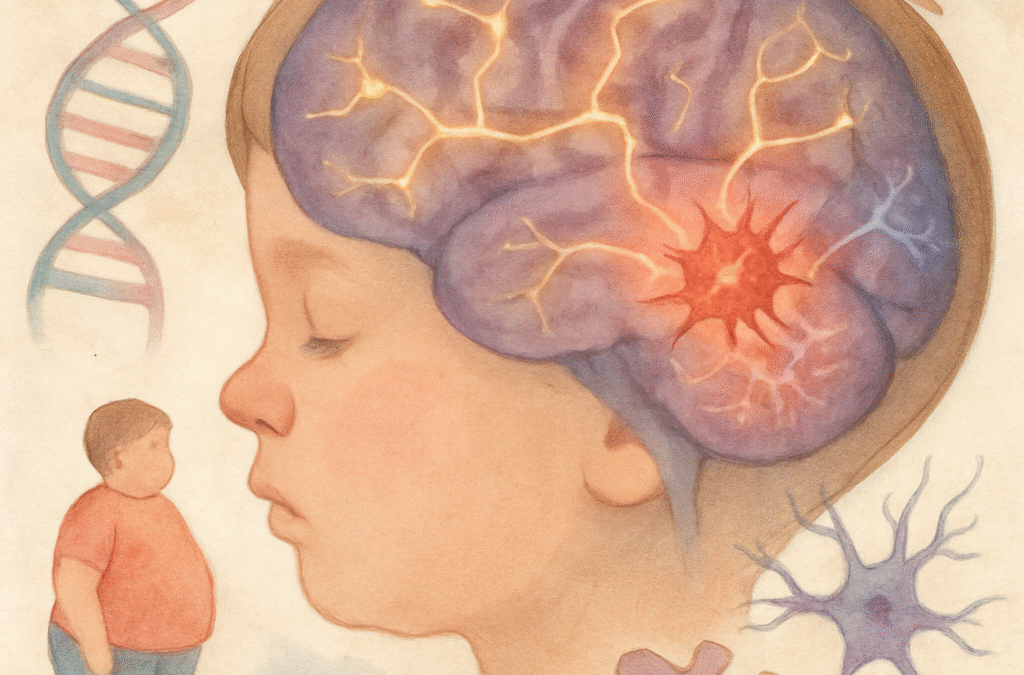
Obesity in childhood is increasingly conceptualised as a brain disease, with compelling evidence demonstrating its deep neurobiological, genetic, and cognitive roots. Scientific studies reveal obesity alters brain structure, function, connectivity, and gene regulation—compromising cognition and mental health not only in youth but also carrying consequences into adulthood (Saeed, Bonnefond, & Froguel, 2024; Tomasi et al., 2024; Wang et al., 2014).
Neurological Mechanisms
Neuroimaging studies in large cohorts show children with obesity exhibit significant reductions in cortical thickness—especially within the prefrontal cortex, critical for executive function and self-regulation (Saeed et al., 2024; Tomasi et al., 2024). MRI data from the Adolescent Brain Cognitive Development (ABCD) study reveal that children with a higher BMI have impaired structural and functional connectivity in networks including the corpus callosum and default mode network, which are central for information integration and cognitive flexibility (Tomasi et al., 2024). Increased spontaneous neural activity in somatomotor regions and decreased connectivity across multimodal association cortices are hallmarks of obesity’s impact on the brain, mediating deficits in attention, reasoning, and overall cognitive composite scores.
Genetic Foundations and Brain Disease Model
Genetic research supports a primary role for the brain in obesity. Over twenty rare gene mutations cause monogenic obesity, and more than a thousand loci are linked to polygenic obesity—most expressed in neural tissues governing appetite, reward, and metabolic regulation (Saeed et al., 2024). Syndromic forms, such as Prader-Willi syndrome, combine developmental delays and severe obesity, reinforcing this brain-based perspective. Maternal obesity and metabolic conditions also impart measurable changes in offspring’s brain structure predisposing to lifelong vulnerability (Tomasi et al., 2024).
Brain Pathways and Neuroendocrine Regulation
The hypothalamus, hippocampus, amygdala, striatum, and prefrontal cortex orchestrate food reward, appetite, and energy balance. In obese children, reward systems are hypersensitive to food cues, but less responsive to satiety signals, producing cycles of overeating and impaired inhibitory control (Tomasi et al., 2024; Saeed et al., 2024). Mutations in leptin-melanocortin pathways, and associated neurohormonal imbalances, account for both profound obesity and cognitive and emotional difficulties.
Impairment of Cognitive Functions
Children with obesity experience pronounced deficits across several cognitive domains. Executive functions—including inhibitory control, planning, and mental flexibility—are consistently compromised. These children struggle more than peers with attention, distraction, resisting impulsive behaviours, and maintaining goal-directed actions, which impacts both academic and personal success (Miller et al., 2015; Sanchez-Castañeda et al., 2021; Tomasi et al., 2024).
Working memory, essential for integrating and recalling information, is reduced in obese children, as is fluid intelligence—the ability to solve novel problems and adapt to change (Tomasi et al., 2024; Wang et al., 2014). They display poorer focus, switching between tasks, and management of complex information, and this decreases further in relation to severity of obesity. Evidence shows that abnormalities in the default mode and precuneus networks hinder self-referential thinking and higher-order reasoning.
Socioeconomic disadvantage can further amplify these cognitive difficulties: children from lower-income families with obesity show more pronounced disruptions in brain connectivity and greater cognitive impairment (Tomasi et al., 2024).
Neurobiological and Epigenetic Mechanisms
Obesity in childhood is associated with chronic low-grade neuroinflammation, hormonal dysregulation, and persistent metabolic stress, adversely affecting brain regions involved in memory and executive function (Saeed et al., 2024; Wang et al., 2014). Mouse models demonstrate that brief early-life exposure to obesity and insulin resistance can induce lasting epigenetic changes—elevated histone deacetylase 5 (HDAC5) and reduced brain-derived neurotrophic factor (BDNF)—which diminish synaptic plasticity and memory consolidation throughout life, even after weight normalises (Wang et al., 2014).
Psychological and Neurodevelopmental Complications
Obese children display higher rates of neurodevelopmental disorders, notably ADHD and learning difficulties, and are more vulnerable to emotional conditions such as anxiety and depression. These comorbidities further complicate the effects of obesity, underscoring the importance of integrated clinical assessment (Hayes et al., 2017; Saeed et al., 2024).
Long-Term Consequences
Experimental and longitudinal studies indicate that childhood and adolescent obesity leave enduring marks on brain architecture and function, posing risks for cognitive decline, impaired learning, and psychiatric disorders in later life (Wang et al., 2014). Restoring healthy body weight does not fully reverse these brain-based changes, highlighting the significance of early prevention.
Implications for Treatment and Prevention
Understanding childhood obesity as a brain disease demands targeted interventions incorporating behavioural, psychosocial, neurocognitive, and medical approaches. Early screening for neurocognitive risk and supportive strategies—such as cognitive training, physical activity, and medications influencing central pathways—show promise in restoring brain health and resilience (Saeed et al., 2024; Tomasi et al., 2024). Tackling poverty and improving cognitive performance in at-risk children are also crucial to reducing obesity risk.
References
Hayes, J. F., et al. (2017). Executive function in childhood obesity. Frontiers in Psychology, 8, 1164.
Miller, A. L., et al. (2015). Obesity-associated biomarkers and executive function in children. Pediatric Research, 78(2), 136–142.
Saeed, S., Bonnefond, A., & Froguel, P. (2024). Obesity: Exploring its connection to brain function through genetic and genomic perspectives. Molecular Psychiatry, 29(7), 1232–1244.
Sanchez-Castañeda, C., et al. (2021). Executive function training in childhood obesity: Food choice, emotional state, and cerebral plasticity. Frontiers in Pediatrics, 9, 551869.
Tomasi, D., et al. (2024). Childhood obesity’s effect on cognition and brain connectivity: Evidence from the ABCD study. JCI Insight, 9(16), e181690.
Wang, J., et al. (2014). Childhood and adolescent obesity and long-term cognitive consequences in adulthood. Journal of Clinical Investigation, 124(12), 5422–5426.